The patient had always been very conscious of her health. She exercised; she was a healthy eater. Then she got a big surprise: she learned that she had been infected with Lyme Disease for the past three years. She didn’t have the classic bullseye rash or symptoms until she suddenly became quite ill.
One of my specialist colleagues at Froedtert South helped her recover from the Lyme Disease, but then her heart started beating irregularly. She was diagnosed with atrial fibrillation, commonly known a-fib. That’s when I met her.
A common cause
A-fib is the most common heart rhythm irregularity, affecting an estimated 2.7 million Americans. It causes the heart to race at up to 120 to 240 beats per minute – many times more than a normal rhythm of 60 to 100 beats per minute.
Picture a still pond. If you drop one drop of water after another into the pond, ripples will emerge outward from that spot. That’s like a normal heart rhythm. A-fib is like it started pouring rain. The ripples and waves go everywhere, colliding and creating chaos in your heart.
That makes people feel very ill and frightened. They’re tired, and can’t do what they want to do because they’re out of breath. They get dizzy and may even pass out. Patients can feel their heart racing and beating irregularly, and that’s extremely unnerving. They think they’re having a heart attack the first time they experience this. People feel just terrible. It often limits what patients can do to practically nothing.
And a-fib can also lead to other more serious health problems. The risk of having a stroke is five times higher. A-fib can also cause a heart attack, or congestive heart failure.

Dr. Indrajit Choudhuri
Calming the chaos
The standard treatment for a-fib is cardiac ablation – a procedure that blocks the electric signals originating in the blood vessels to the lungs that enter the heart and cause it to beat erratically. Here at Froedtert Pleasant Prairie Hospital, we perform ablations using a leading edge, non-invasive procedure called pulmonary vein isolation, or PVI.
A catheter is inserted into a vein in the patient’s groin. A camera and a balloon with a tiny laser are inserted through the catheter. I can look right at the areas where the pulmonary veins connect with the heart. I make sure the balloon is positioned correctly, then activate the device. In about two minutes I’ve isolated the whole vein, blocked the errant electrical signals, and halted the a-fib.
That’s a big advance. We’ve gone from many hours of making lesions, one at a time, to positioning a balloon with an automated laser to travel around the pulmonary vein and achieve what we want quickly and accurately in minutes.
Patients are benefitting from these shorter procedure times. They have excellent outcomes. After I performed the PVI procedure on my Lyme Disease patient, her blood pressure and heart rate went back to normal immediately. She went home the next day, and quickly returned to exercising and gardening without feeling so tired and out of breath.
It’s also a very safe procedure for patients because they avoid being exposed to radiation or having to be under general anesthesia for an extended period of time. There are still some risks that cannot be completely eliminated, but I have the entire resources of the hospital system at my disposal if a complication arises.
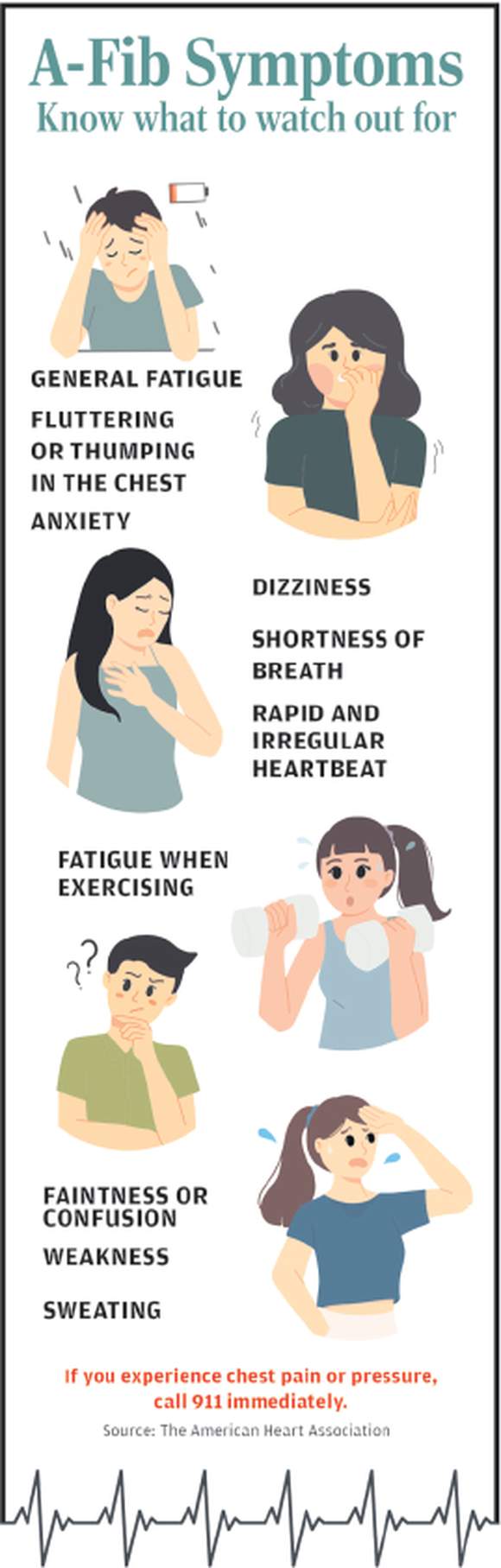
A-fib Symptoms
Lower risk of stroke with higher quality of life
With a-fib, there are two main issues that we have to deal with: One is the faulty heart rhythm itself, which we address with medicines or ablation.
The other is the risk of stroke. To lower that risk, we put patients on blood thinners, often for the rest of their lives. With more and more people developing a-fib in their fifties and sixties – and then living into their seventies, eighties, and even nineties – some patients could be on blood thinners for ten, twenty, or even thirty years, required to have their blood tested every two to four weeks for decades.
Also, if a patient taking blood thinners nicks themself shaving, they may bleed excessively. If they accidentally bump into something, they may bruise an entire arm or leg. Blood thinners can even cause severe bleeding in the brain or gastrointestinal tract, requiring hospitalization, emergency surgery, and blood transfusions. All this can dramatically reduce an a-fib patient’s quality of life. That’s why we are all very excited about the new Watchman Program that we’re starting this summer.
With the Watchman procedure, we use a catheter to place a small inflatable disc into what’s called the left atrial appendage of an a-fib patient’s heart – an area of their heart where a-fib can cause blood clots to form. The disc prevents blood clots from forming – eliminating the danger that they could travel to the brain and cause a stroke. The procedure typically takes only an hour or less to perform, but it has a big impact on a-fib patients, by giving us a way to lower their risk of stroke without requiring them to take blood thinners for the rest of their lives.
Breakthrough care close to home
Here at Froedtert South, we have the fastest growing complex ablation program in southeast Wisconsin, with the most advanced imaging, mapping, and electrophysiology navigation systems available. Our staff is absolutely incredible. They love being part of a team that’s really helping people.
It’s an extraordinarily rewarding experience to be able to use these leading-edge technologies and our expertise to provide the absolute highest level of cardiac electrophysiology care to patients. We are here, close to home, ready to give the people of this community what we believe they deserve: the very best in breakthrough cardiac care.
