Dr. Fullin holds the Medtronic Micra pacemaker.
Wireless pacemakers, temporary heart pumps and dyeless digital imaging.
In the assessment of medical professionals, this is “an exciting time” to be working in cardiology.
In recent months three very new devices and technical innovations have been implemented by Dr. Kevin Fullin, interventional cardiologist and the heart team at Froedtert South.
Micra: the world’s smallest pacemaker
Last fall, Fullin implanted a tiny wireless pacemaker known as the Micra Transcatheter Pacing System.
Approved by the FDA for use in 2016, this is a 1-inch-long device about the size of a vitamin capsule. Where conventional pacemakers consist of a transmitting device plus one to three wire leads, the Micra is an all-in-one unit.
“Traditional pacemakers have helped a tremendous amount of patients keep their heart rates from going too slow and restarting their hearts,” Fullin said.
On the other hand, he said, “the leads move with every heartbeat, and so with time they can fracture, and then we have to put a new lead in.”
Another downside to wire leads is a susceptibility to contamination from viruses in the body. In this case, the wires have to be removed and replaced.
Other problems might include in-vessel bleeding, or in very rare cases a punctured lung during implant surgery.
The Micra bypasses all of these issues, so to speak.
Inserted via a catheter from the groin, the enclosed tube containing a battery and pacing device has four tiny flexible anchors that attach to the fibrous tissue of the heart.
“Once we confirm it is pacing well and anchored well, it detaches it from the catheter,” Fullin said.
The Micra lasts 15 years; traditional pacemakers last 10.
“A bonus fact is that because the Micra is so small, in the event it needs replacing, the surgeon won’t remove the first one, but can leave it in and just add a new one right next to it,” Fullin said.
Fullin said the Micra will be particularly helpful for patients for whom pacemaker lead infection has been an issue or for those with already infected pacemakers.
The current generation of the Micra only paces in one chamber and so will be used only for patients who need only a single chamber to be paced.
While standard pacemakers can pace more than one chamber, additional wire leads are required for each chamber that is paced.
“(The Micra) is ideal for patients who have something like ulcerated sores somewhere on the body and can’t risk getting the infection transferred onto pacemaker leads,” Fullin said.
“We are very excited about this because this is safer for some patients where the risk of these other things is very high,” Fullin said.
CO2 imaging
Another innovation is aortic imaging.
To see what’s going on inside the heart and its vessels in real time, cardiologists have used contrast injection with digital imaging in a procedure known as angiography.
Traditionally this is done using a contrast media or dye that travels through the body’s vein network. This dye, however, can be hard on the kidneys to process.
Finding a way to get those same real-time pictures without dye has become another exciting boon to cardiology, say experts.
Last fall, Fullin and the heart team stented a kidney artery using CO2 imaging, a process involving the injection of a small amount of carbon dioxide rather than dye into the patient’s system.
“With this patient we suspected blockage in the kidney arteries. But to see it, we would need to use dye, but that would make it worse. We could have used medication to try to prevent this (side effect) but better yet to use (CO2 imaging),” Fullin said.
Using the CO2mmander from AngioAdvancements, the surgical team was able to capture the needed images using only 10 cc of CO2 where with dye they would have had to administer a 120 cc dose.
“10 cc doesn’t hurt the kidney; 120 cc does,” he said.
Fullin said that physicians have known for a long time that CO2, a component of air, could provide contrast images. Eventually the technology developed by which CO2 could be compressed, packaged and utilized.
“Air, which is a mixture of gases, would be lethal if injected into the body; pure carbon dioxide, however, is absorbed by the tissues,” he said.
Carbon dioxide angiography is especially helpful to patients with “fairly common” conditions including, kidney damage, leg arteries and leg aneurysms, Fullin said.

Dr. Fullin and Dr. Sanborn discussing recent technology improvements.
Impella pump
Last but not at all least is a temporary heart pump used to stabilize patients in emergency heart attack situations.
Known as the Impella Support system by Abiomed, the small device pumps blood into the aorta to rest the heart muscle and stabilize patient blood pressure while the surgeon addresses the problem.
Since last fall, Fullin has performed several cases of high-risk coronary procedures using the pump.
“They are considered high risk because the muscle is weakened (by heart attack), and then patients don’t have much reserve (muscle strength) which makes doing angioplasty risky,” Fullin said.
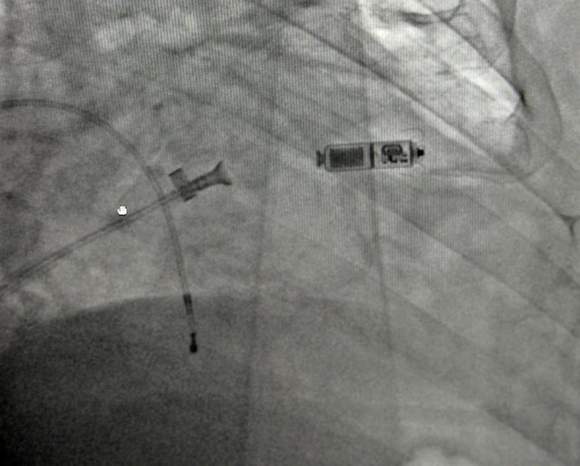
Dr. Fullin demonstrates how the Micra pacemaker (small object right) looks after placement in a patient.
The Impella heart pump is temporarily placed in the left ventricle of the heart. Using an Archimedes Screw type pump devised by the late cardiac pioneer Dr. Michael DeBakey, the device pumps blood into the aorta to rest the heart muscle stabilizing blood pressure and allowing other organs such as the kidneys to function better as well, Fullin said.
Before Impella, surgeons used an intraaortic balloon pump timed with the cardiac cycle.
“The Impella is believed to be so much more effective because it decreases (heart) wall stress and thus the work load of the ventricle,” Fullin said. “It is particularly good for use with patients who have had multiple heart procedures.”
After the surgeon performs the angioplasty and/or implants stents, the pump is removed.
“The Impella pump is a game changer. ... For so long mortality rates were so high from (cardiogenic) shock,” Fullin said.
To date, three procedures have been done at Froedtert using the Impella pump.
“The results are really inspiring,” Fullin said.
Dr. Timothy Sanborn, medical director and chairman of cardiothoracic services at Froedtert South, is also enthusiastic about the technological advances and implementations.
“The new devices and technology have exponentially improved patient care,” he said.
Citing statistics, Sanborn noted, “(Mortality) used to be as high as 90 percent before we started using techniques like angioplasties and stents. With those developments it went down to 50 percent and now (the Impella) brings it down to 25 percent.”
“That’s progress,” he said. “(More) people are now alive.”
Asked what drives the pursuit of the latest technologies, Fullin said, “Changes in mortality rates make it worthwhile to do.”